CDKL5 Deficiency Disorder: Frontiers of Disease Modifying Therapy and Promising Visual Outcome Measures
By Heather Olson, MD, MS
Assistant Professor of Neurology
Director, CDKL5 Clinic
Boston Children’s Hospital and Harvard Medical School
CDKL5 Deficiency Disorder (CDD) is an X-linked developmental and epileptic encephalopathy presenting in females and males with a ratio of approximately 4:1.1 CDD has an estimated prevalence of one in 40,000 to 60,000 live births.1 CDKL5 is one of the genes for which disease-associated variants are most commonly identified on epilepsy gene panels, and there is additionally a high rate of somatic mosaicism especially in males.2-4 Seizures typically present in the first 3 months of life, and associated features include hypotonia, severe global developmental delay with or without regression, intellectual disability, cerebral visual impairment, sleep and gastrointestinal disturbances.1 Variable features include dysphagia, autonomic abnormalities and dyskinetic movements.1
Boston Children’s H ospital (BCH) is one of eight CDKL5 Centers of Excellence supported by the International Foundation for CDKL5 Research. The CDKL5 Centers of Excellence and the International CDKL5 Disorder Database joined efforts to create the International CDKL5 Clinical Research Network (ICCRN), with a combined database. At BCH we have an extensive basic and translational research program to study CDKL5-related disease. See key BCH collaborators for basic, translational, and clinical research in the blue side box.
ospital (BCH) is one of eight CDKL5 Centers of Excellence supported by the International Foundation for CDKL5 Research. The CDKL5 Centers of Excellence and the International CDKL5 Disorder Database joined efforts to create the International CDKL5 Clinical Research Network (ICCRN), with a combined database. At BCH we have an extensive basic and translational research program to study CDKL5-related disease. See key BCH collaborators for basic, translational, and clinical research in the blue side box.
Promise of Disease Modifying Therapy
CDD is highly refractory to current treatments for epilepsy.1 This includes worse responses to first line medications for infantile spasms than in other etiologies (controls from the National Infantile Spasms Consortium database).1, 5 Ganaxolone is the first medication that has shown positive response in phase 3 clinical trials.6 In addition, fenfluramine and cannabidiol have demonstrated improvement in seizures counts in small phase 2 clinical trials7, 8 while other small molecule trials have been completed or planned. Disease modifying therapies including viral-based gene therapy, gene editing, escape of X-inactivation, and ASO approaches are in various stages of development. Early proof of concept protein and gene replacement therapy in mouse and induced pluripotent stem cell models has been promising but these therapies are not yet ready for human trials.9-11
Visual Outcomes
 While awaiting these promising disease-modifying therapies, our CDKL5 Centers of Excellence are working to establish and validate clinical outcome measures. Seizure counts, while beneficial for medications targeting seizures, do not adequately capture overall disease severity. In fact, families prioritize alertness and interaction at least as highly as seizure control, and symptoms related to sleep and gastrointestinal disorders are high on their list of quality-of-life concerns.
While awaiting these promising disease-modifying therapies, our CDKL5 Centers of Excellence are working to establish and validate clinical outcome measures. Seizure counts, while beneficial for medications targeting seizures, do not adequately capture overall disease severity. In fact, families prioritize alertness and interaction at least as highly as seizure control, and symptoms related to sleep and gastrointestinal disorders are high on their list of quality-of-life concerns.
In CDD, communication is particularly challenging because of poor hand function and poor visual function. Improvement in these abilities would open opportunities for picture-based augmentative communication, via touch or eye gaze, giving families an improved pathway for interacting with their child.
To enable us to assess the range of disease severity in CDD, change over time, and ultimately measure effectiveness of disease modifying therapies, we have developed a disease-specific CDKL5 Severity assessment, and completed content validation of the clinician portion of this assessment.12, 13 Our eight Centers of Excellence, with Colorado as the lead site, have received NINDS funding for a clinical trial readiness grant, with the purpose of, establishing a suite of clinical outcome measures and investigating visual and sensory evoked potentials and quantitative EEG as biomarkers (1U01NS114312-01A1).
Cerebral Visual Impairment Phenotype: One of the key recognized features of CDD is prominent cerebral visual impairment, therefore, visual function is included in the disease-specific CDKL5 Severity assessment.1, 12-15 Visual outcome measures may be considered in future clinical trials when relevant. At BCH we were able to characterize the visual phenotype based on clinical data from ophthalmological and neurological assessments.14 The visual phenotype is consistent with cerebral visual impairment, which was diagnosed in all individuals over the age of 2 years in our study.14
KEY BCH COLLABORATORS
Collaborative projects at BCH include but are not limited to the following:*
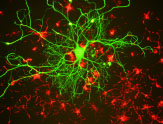
- CDKL5 mouse models in the lab of Michela Fagiolini with projects including behavioral and visual characterization;
- Patient-derived fibroblast and iPSC lines collected from clinic that are being characterized through the Human Neuron Core and Mustafa Sahin’s laboratory;
- Connectivity and tractography projects in mouse and humans (Michela Fagiolini’s laboratory, Jurriaan Peters, Heather Olson and the neuroimaging core);
- Proof of concept anti-sense oligonucleotide (ASO) development as a collaborative effort between Tim Yu’s laboratory, Michela Fagiolini’s laboratory and Heather Olson’s clinical research program;
- Investigation of CDKL5’s role in the corpus callosum (Hisashi Umemori’s laboratory); and,
- Biomarker development including sensory evoked potentials and high-density EEG (Charles Nelson’s laboratory in collaboration with Heather Olson’s clinical research program, part of multi-site efforts with Eric Marsh at Children’s Hospital of Philadelphia as a lead investigator).
*Bolded investigators are members of the Intellectual and Developmental Disabilities Center at Boston Children’s Hospital.
Visual Acuity Outcome Measures
In our trials visual acuity, measured by preferential looking test and sweep visual evoked potential (sVEP), was below population controls.14 Results of the preferential looking test, showed that acuity correlated with gross motor function (ability to mobilize with or without support).14 A greater than 1 octave gap of sVEP acuity, higher than preferential looking acuity, was consistent with diagnosis of cerebral visual impairment.14
We propose, based on our initial clinical data, that measurements of visual acuity, including the preferential looking test and sVEP may serve as quantifiable outcome measures with relationship to the developmental status. In our small series it was statistically correlated with gross motor ability. We hypothesize that we would identify more broadly a relationship of visual acuity with developmental status and disease severity in a larger prospective study. Further work is needed to validate these tools as outcome measures and assess relationship to disease severity, seizures, medications and other clinical factors. A study from the University of Colorado will be published soon demonstrating use of a novel clinical cerebral visual impairment score, another approach to assess visual function in this population.
Through collaboration with Dr. Charles Nelson’s laboratory, we have performed visual and auditory evoked potentials (VEPs, AEPs) in children with CDD as part of the Rett and Related Disorders Natural History study and support from the International Foundation for CDKL5 Research. This work will be expanded through a biomarker component of the clinical trial readiness grant for CDD (1U01NS114312-01A1), for which we are one of three sites performing biomarker studies. Further work is needed to assess variability and relationship to disease severity using a disease-specific tool.
Visual outcome measures have not traditionally been considered in developmental disorders, but evidence of abnormalities in VEPs in Rett syndrome and relationship to overall disease severity has set a precedent for this work.16, 17 Vision outcome measures have additionally been used in other neurologic disease including Multiple Sclerosis.18
Please watch for our work on CDKL5 Deficiency Disorder.
Thank you to the IDDRC for supporting our collaborative efforts spanning clinical, translational and basic science at BCH as well as national and international collaborations.
References
- Olson HE, Demarest ST, Pestana-Knight EM, et al. Cyclin-Dependent Kinase-Like 5 Deficiency Disorder: Clinical Review. Pediatr Neurol. 2019 Aug;97:18-25.
- Lindy AS, Stosser MB, Butler E, et al. Diagnostic outcomes for genetic testing of 70 genes in 8565 patients with epilepsy and neurodevelopmental disorders. Epilepsia. 2018 May;59(5):1062-71.
- Stosser MB, Lindy AS, Butler E, et al. High frequency of mosaic pathogenic variants in genes causing epilepsy-related neurodevelopmental disorders. Genet Med. 2018 Apr;20(4):403-10.
- Symonds JD, McTague A. Epilepsy and developmental disorders: Next generation sequencing in the clinic. Eur J Paediatr Neurol. 2020 Jan;24:15-23.
- Olson HE, Demarest S, Pestana-Knight E, et al. Infantile spasms in CDKL5 deficiency disorder respond poorly to first line treaments. American Neurological Association Annual Meeting. 2020;2020-NINA-86-ANA.
- Pestana-Knight E, Amin S, Benke TA, Cross JH, Olson HE, Specchio N. Ganaxolone significantly reduces major motor seizures associated with CDKL5 deficiency disorder: A randomized, double-blind, pacebo-controlled phase 3 study (Marigold Study). American Epilepsy Society Annual Meeting. 2020.
- Devinsky O, Cross JH, Laux L, et al. Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N Engl J Med. 2017 May 25;376(21):2011-20.
- Devinsky O, King L, Schwartz D, Conway E, Price D. Effect of fenfluramine on convulsive seizures in CDKL5 deficiency disorder. Epilepsia. 2021 Jul;62(7):e98-e102.
- Gao Y, Irvine EE, Eleftheriadou I, et al. Gene replacement ameliorates deficits in mouse and human models of cyclin-dependent kinase-like 5 disorder. Brain. 2020 Mar 1;143(3):811-32.
- Trazzi S, De Franceschi M, Fuchs C, et al. CDKL5 protein substitution therapy rescues neurological phenotypes of a mouse model of CDKL5 disorder. Hum Mol Genet. 2018 May 1;27(9):1572-92.
- Benke TA, Kind PC. Proof-of-concept for a gene replacement approach to CDKL5 deficiency disorder. Brain. 2020 Mar 1;143(3):716-8.
- Demarest S, Pestana-Knight EM, Olson HE, et al. Severity Assessment in CDKL5 Deficiency Disorder. Pediatr Neurol. 2019 Aug;97:38-42.
- Saldaris J, Weisenberg J, Pestana-Knight E, et al. Content Validation of Clinician-Reported Items for a Severity Measure for CDKL5 Deficiency Disorder. J Child Neurol. 2021 Oct;36(11):998-1006.
- Olson HE, Costantini JG, Swanson LC, et al. Cerebral visual impairment in CDKL5 deficiency disorder: vision as an outcome measure. Dev Med Child Neurol. 2021 May 24.
- Demarest ST, Olson HE, Moss A, et al. CDKL5 deficiency disorder: Relationship between genotype, epilepsy, cortical visual impairment, and development. Epilepsia. 2019 Aug;60(8):1733-42.
- LeBlanc JJ, DeGregorio G, Centofante E, et al. Visual evoked potentials detect cortical processing deficits in Rett syndrome. Ann Neurol. 2015 Nov;78(5):775-86.
- Saby JN, Benke TA, Peters SU, et al. Multisite Study of Evoked Potentials in Rett Syndrome. Ann Neurol. 2021 Apr;89(4):790-802.
- Balcer LJ, Raynowska J, Nolan R, et al. Validity of low-contrast letter acuity as a visual performance outcome measure for multiple sclerosis. Mult Scler. 2017 Apr;23(5):734-47.



